Archive for the ‘Plain City Health’ Category
Understanding Depression: Medication, Lifestyle Changes, and Environmental Factors. By Our Student Pharmacist Deema Alhaj.
Depression is a complex mental health condition affecting millions of people worldwide. It can manifest as persistent feelings of sadness, hopelessness, and loss of interest in activities once enjoyed. Fortunately, there are various treatment options available, including medication, lifestyle changes, and environmental factors, which can help individuals cope with and manage depression effectively.
Medication can be an essential component of depression treatment, especially for individuals with severe or persistent symptoms. Antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), work by balancing neurotransmitters in the brain. Neurotransmitters help improve mood and alleviate depressive symptoms.
In addition to medication, lifestyle modifications can significantly impact one’s mental health and well-being, and it’s important for patients to work on improving their lifestyle such as:
- Balanced Diet: Eating a well-balanced diet with plenty of fruits, vegetables, whole grains, and lean proteins provides essential nutrients that support brain health. Omega-3 fatty acids found in fish have shown promise in alleviating depression symptoms.
- Regular Exercise: Engaging in physical activities like walking, jogging, or yoga promotes the release of endorphins, the “feel-good” hormones. Exercise has been shown to reduce symptoms of depression and improve overall mood.
- Sufficient Sleep: Sleep plays a vital role in emotional regulation and cognitive function. Adopting good sleep hygiene practices can improve sleep quality and help manage depressive symptoms.
- Mindfulness and Meditation: Practicing mindfulness and meditation techniques can help individuals gain better control over negative thought patterns and reduce stress.
Environmental factors can both contribute to and mitigate depression. Understanding and addressing these factors is crucial for managing the condition:
- Social Support: A strong social support system can serve as a buffer against depression. Positive relationships with friends, family, or support groups provide emotional validation and reduce feelings of isolation.
- Stressful Life Events: Experiencing traumatic or stressful life events, such as loss, financial difficulties, or job-related stress, can increase the risk of depression. Coping mechanisms and resilience play vital roles in managing these stressors.
- Physical Environment: Living in a safe and supportive environment can positively impact mental health. Access to green spaces, natural light, and a clutter-free living space can create a more positive atmosphere.
Conclusion: Depression is a multifaceted condition that requires a comprehensive approach to treatment. Medication, lifestyle changes, and addressing environmental factors can significantly improve one’s ability to manage and cope with depression. However, it is essential to remember that individual responses to treatment may vary, and seeking professional help is crucial for personalized and effective treatment.
Remember, you are not alone. Reach out for support from loved ones or mental health professionals if you or someone you know is experiencing depression. With the right strategies and support, individuals can lead fulfilling lives, even in the face of depression.
References:
- Medication for Depression:
- National Institute of Mental Health (NIMH). (2021). “Depression.” Retrieved from: https://www.nimh.nih.gov/health/topics/depression/index.shtml
- Khan A, Faucett J, Lichtenberg P, Kirsch I, Brown WA (2012) A Systematic Review of Comparative Efficacy of Treatments and Controls for Depression. PLoS ONE 7(7): e41778. https://doi.org/10.1371/journal.pone.0041778
- Lifestyle Changes to Combat Depression:
- Harvard Health Publishing. (2021). “Exercise is an all-natural treatment to fight depression.” Retrieved from: https://www.health.harvard.edu/mind-and-mood/exercise-is-an-all-natural-treatment-to-fight-depression
- Smith, P. J., Blumenthal, J. A., Hoffman, B. M., Cooper, H., Strauman, T. A., Welsh-Bohmer, K., Browndyke, J. N., & Sherwood, A. (2010). “Aerobic exercise and neurocognitive performance: a meta-analytic review of randomized controlled trials.” Psychosomatic Medicine, 72(3), 239-252. doi: 10.1097/PSY.0b013e3181d14633
- Environmental Factors and Depression:
- Cohen, S., Underwood, L. G., & Gottlieb, B. H. (2000). “Social Support Measurement and Intervention: A Guide for Health and Social Scientists.” Oxford University Press.
- Grinde, B., & Patil, G. G. (2009). “Biophilia: Does Visual Contact with Nature Impact on Health and Well-Being?” International Journal of Environmental Research and Public Health, 6(9), 2332-2343. doi: 10.3390/ijerph6092332
- Front. Psychol., 02 September 2020
Sec. Health Psychology Volume 11 – 2020 | https://doi.org/10.3389/fpsyg.2020.588604
Preventing Tick Bites: Tips for Enjoying the Outdoors Safely. By Our Student Pharmacist, Lee Zimmer.
This may be biased, but summers in Ohio are simply the best, that is, when it isn’t storming or blisteringly hot. As the summer season unfolds in central Ohio, many people may be eager to embrace the great outdoors and enjoy the amazing trails and metro parks around us. However, before you run out the door and start doing cartwheels, we should have a quick discussion about one of the potential health risks this season – tick bites. Ticks can carry diseases like Lyme disease and Rocky Mountain Spotted Fever and can pose a threat to not just our well-being, but to our pets as well. Forewarned is forearmed as they say, so don’t fret! In this blog post, we’ll provide you with valuable tips to prevent tick bites, ensuring you can safely enjoy your outdoor adventures.
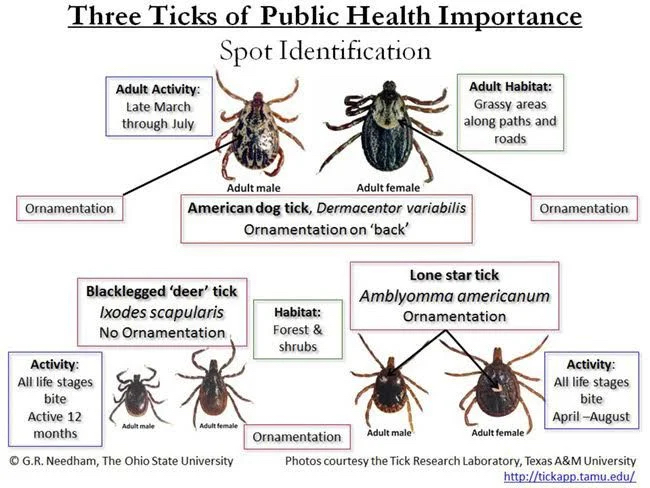
- Know Your Enemy: Understanding Ticks and Their Habitats
To effectively prevent tick bites, it’s crucial to familiarize yourself with these tiny arachnids.
The three medically important tick species in Ohio are the:
- American dog tick
- Blacklegged tick (aka Deer tick)
- Lone Star tick
While some species can actually remain active throughout the entire year, the time of greatest activity for most tick species is from spring to fall. The American dog tick inhabits grassy areas along roads or paths, often next to wooded areas. The Blacklegged tick prefers wooded areas, while the Lone Star tick loves shady areas next to meadows and roadsides.
- Dress to Repel: Tick-Proof Clothing Choices
Wearing the right clothing can act as a barrier against ticks. Opt for long-sleeved shirts, long pants, and closed-toe shoes whenever possible. Tuck your pants into your socks or boots to minimize exposed skin. Additionally, choose light-colored clothing to spot ticks more easily.
- Tick Repellents: Safeguarding Your Skin
Apply an EPA-approved tick repellent to exposed skin and clothing. Look for products containing DEET (25% minimum), picaridin, or permethrin. Follow the instructions carefully, ensuring thorough coverage. Remember to reapply as recommended, especially if you’re engaging in prolonged outdoor activities.

- Tick-Proof Your Yard: Creating a Tick-Unfriendly Environment
Make your yard less appealing to ticks by implementing a few simple measures:
- Trim grass and vegetation regularly.
- Keep leaf litter and brush cleared.
- Create a barrier of wood chips or gravel between your yard and wooded areas.
Consider professional pest control treatments if necessary.
- Conduct Tick Checks: Thoroughly Inspect Yourself and Others
After spending time outdoors, perform a thorough tick check on yourself, family members, and pets. Pay close attention to warm areas like armpits, behind the ears, along the hairline, and between toes. Promptly remove any attached ticks using fine-tipped tweezers, grabbing as close to the skin as possible (you want to get the WHOLE tick), and clean the area with antiseptic.
Side note, please don’t attempt to burn ticks off of yourself or someone else. It feels pretty self-explanatory why that is a bad idea, but it needed said.
- Protect Your Pets: Tick Prevention for Furry Friends
Ticks pose a significant risk to our beloved pets. Consult your veterinarian to determine the most appropriate tick prevention methods for your furry companions. Options may include tick collars, topical treatments, or oral medications. Regularly inspect and groom your pets to catch any hitchhiking ticks.
- Educate Yourself: Recognizing Tick-Borne Diseases
Familiarize yourself with the signs and symptoms of tick-borne diseases prevalent in Ohio, such as Lyme disease spread by the Blacklegged tick. The Centers for Disease Control and Prevention (CDC) state that ticks need to be attached for 24 hours or more to transmit disease. If you experience any unusual symptoms (like fever or flu-like symptoms) within a few weeks of a tick bite, contact your health care provider and emphasize that you were recently bitten by a tick.
 With the right knowledge and preventive measures, you can enjoy the summer season while minimizing the risk of bites from these little blood suckers (and mosquitoes too, but that’s another topic for another day). Add these tips into your outdoor routine, educate others about tick prevention, and remember to check yourself and others.
With the right knowledge and preventive measures, you can enjoy the summer season while minimizing the risk of bites from these little blood suckers (and mosquitoes too, but that’s another topic for another day). Add these tips into your outdoor routine, educate others about tick prevention, and remember to check yourself and others.
Tick-related concerns shouldn’t prevent you from experiencing the warm weather while we have it, so get out there and hit the trails or amble through the parks and green spaces we are lucky to have around us. Stay safe, stay informed, and savor every moment!
For more information on ticks, check out the CDC’s website: https://www.cdc.gov/ticks/
For information about central Ohio Metro Parks, including maps and events, check out: https://www.metroparks.net/
Celiac Disease and Gluten. By Our Student Pharmacist, Niket Patel.
Have you ever wondered, what even is gluten? Today, I will aim to answer that question and talk about celiac disease.
Gluten is a protein found in wheat, rye, barley, and more. It acts as a glue and helps food maintain its structure. Therefore, gluten can be found in many foods you may not expect.
Here are some examples:
- Breads
- Cereals
- Pasta
- Sauces and salad dressings
- Malt milkshakes
- Beer
- Oats
Some individuals may have celiac disease if they are sensitive to gluten. Celiac disease is a serious autoimmune condition where eating gluten damages the small intestine in your stomach. The small intestine has small brush like projections called villi that help your body absorb nutrients. In people with celiac disease, the body reacts to gluten such that it damages these villi and decreases the body’s ability to absorb nutrients.

It is important to note that celiac disease is genetic and people with a first degree relative (parent, child, sibling) have a 1 in 10 risk of developing celiac disease.
High risk factors for celiac disease include:
- type 1 diabetes
- irritable bowel syndrome
- other autoimmune diseases
Symptoms can start to appear because of stress, pregnancy, surgery, or infection.
Symptoms include:
- Constant constipation or diarrhea
- Abdominal pain
- Weight loss
- Gas
- Pale, bad smelling stool
- Unexplained low blood count that makes you feel tired (anemia)
- Tingling, numbness in the legs
- Muscle cramps or joint pain
Untreated celiac disease can lead to heart disease, small bowel cancers, and other autoimmune conditions such as diabetes. Celiac disease can be diagnosed at any age and earlier diagnosis lowers the chance of developing another condition.
The most accurate way to diagnose celiac disease is by a biopsy; a long thin tube is directed through your mouth down to your stomach and into your small intestine. A tool is then passed through the tube to take a tissue sample which is tested in a lab.
Unfortunately, the only treatment for celiac disease is a strict gluten-free diet. This must be a life-long lifestyle change to prevent damage to the small intestine. The good news is that taking gluten out of your diet usually starts to heal your intestine and improves symptoms within a few days!
Eliminating gluten may be difficult, but patients can still enjoy a variety of great foods!
Patients with celiac disease should base their diet around:
- Fruits
- Vegetables
- Meats
- Fish
- Beans
- Legumes
- Nuts
If you are concerned about the safety of a grain, purchase ones that are tested for gluten and contain less than 20 parts per million (ppm). Gluten free bread can usually be found in the freezer section and there are gluten-free flours and flour blends available to bake your own bread.
It is important to note that “wheat-free” does not mean “gluten-free”, so make sure to be careful when reading labels and use the resources linked below to learn more!
References:
- What is celiac disease? Celiac Disease Foundation. Accessed July 18, 2023. https://celiac.org/about-celiac-disease/what-is-celiac-disease/.
- professional CC medical. Celiac disease: Symptoms & how it’s treated. Cleveland Clinic. Accessed July 18, 2023. https://my.clevelandclinic.org/health/diseases/14240-celiac-disease.
- Celiac disease. JHM. Accessed July 18, 2023. https://www.hopkinsmedicine.org/health/conditions-and-diseases/celiac-disease
Supporting Local Farmers: Fresh and Healthy Produce in Columbus and Central Ohio. By Our Student Pharmacist, Lee Zimmer.
As any gardener can attest, the growing season from Spring to Fall can be one of the most labor intensive and rewarding times of the year, but getting to enjoy the fruits of the garden is priceless. That said, most backyard hobby gardens are small potatoes (pardon the pun) when it comes to what our local farmers can bring to the table, and your plate.
In the Columbus and Central Ohio area, we are fortunate to have a vibrant agricultural scene, with numerous farmers’ markets and farm-to-table initiatives. In this blog post, we’ll explore the benefits of buying fresh produce from local farmers, share tips for navigating farmers markets, and highlight the positive impact of supporting our local food system.
- Taste the Difference: Fresher and Flavorful Produce
One of the most compelling reasons to support local farmers is the superior taste of their produce. Unlike mass-produced fruits and vegetables that often travel long distances, local produce is harvested at peak ripeness and arrives at your table within a short time frame. The result? Crisp, vibrant flavors that elevate your culinary experience.
- Nutritional Powerhouse: Maximize Health Benefits
Freshly picked local produce retains its nutritional value better, packing a punch of vitamins, minerals, and antioxidants. By purchasing from local farmers, you ensure that you’re getting the maximum health benefits from your fruits and vegetables. Incorporating these nutrient-rich foods into your diet helps promote overall well-being and boosts your immune system.
- Seasonal Delights: Embrace Variety and Culinary Creativity
Supporting local farmers means embracing the beauty of seasonal eating. Farmers markets showcase an array of produce that changes with the seasons, allowing you to discover new flavors and experiment with diverse ingredients. From juicy blueberries in summer to crisp apples in the fall, each season offers a fresh bounty of options to savor and enjoy.
- Know Your Food: Building Trust and Transparency
Connecting with local farmers fosters a deeper understanding of where your food comes from. Many farmers are passionate about sustainable and organic practices, prioritizing the well-being of both the land and consumers. Don’t be intimidated; they actually want to talk to you about their practices and products, so ask questions, gain insight, and build trust in the food you consume.
- Boosting the Local Economy: Supporting Community Resilience
Every dollar spent at a local farmers market goes directly back into the community, supporting the livelihoods of farmers, their families, and the local economy. By choosing local produce, you contribute to the sustainability and resilience of your community, creating a ripple effect that benefits everyone.
- Environmental Stewardship: Reducing Food Miles and Waste
Buying locally grown produce reduces the carbon footprint associated with long-distance transportation. By supporting local farmers, you help minimize food miles, conserve energy, and mitigate climate change. Additionally, local produce is less likely to be wasted, as it doesn’t need to endure extensive transportation and storage.
- Explore the Variety: There’s More to the Market
I would be remiss to not include that farmers markets go beyond fruits and veggies! Oftentimes you can find stands specializing in locally produced meats, cheeses, baked goods, and other favorites – like fresh local honey and plants to add to the garden. You never know what you might stumble across or what may inspire you to try something new.
Make the most of your farmers market experience with a few handy tips:
- Arrive early for the best selection.
- Bring reusable bags and containers. Most may have bags, but it’s better safe than sorry.
- Don’t hesitate to strike up conversations with farmers. They can offer recommendations, cooking tips, and even inspire new recipe ideas.
- Embrace the vibrant atmosphere and immerse yourself in the local food culture.
- Explore different markets in different areas; oftentimes you’ll find other vendors that are not at your local market.
Supporting local farmers is a great way to savor fresh, healthy, and flavorful goods while making a positive impact on your community. By choosing to buy from local farmers, you embrace seasonal variety, enhance your well-being, and contribute to a resilient and sustainable food system.
So, visit your nearest farmers market, connect with local growers, and enjoy the abundant goodness that local produce has to offer!
- Plain City’s Farmers Market
The Plain City Farmers Market is held every Thursday from 4:30 to 7 pm until October 5 in the flatiron (101 South Chillicothe Street) of uptown Plain City located beside the clock tower building.
For more information, visit their Facebook page HERE.
- Jacquemin Farms
Jacquemin Farms on 7437 Hyland-Croy Road in Plain City offers a farm market that is open Monday to Friday from 9 am to 6 pm, Saturday, 9 am to 5 pm. They also have a wonderful bakery that is open Tuesday-Saturday 7 am-2 pm and incorporates their fresh veggies and fruits into the menu.
Visit their Facebook page HERE.
- Yutzy’s Farm Market
Yutzy’s Farm Market is located at 6010 Converse Huff Road in Plain City and brings the produce of local farmers to their farm market. They are open Monday through Saturday, 9 am to 5 pm, closed Sundays.
Visit their web site HERE or their Facebook page HERE.
For a list of local farmers markets, locations, days, and times, check out Experience Columbus’ website: https://www.experiencecolumbus.com/things-to-do/shopping/farmers-markets/
New Long-Acting Insulin for Diabetics Will Help Reduce Pokes and HbA1c. By Our Student Pharmacist, Niket Patel.
If you or someone you know uses long-acting or basal insulin to manage their diabetes, there may be a more convenient option available for you soon!
Today, I am highlighting some positive clinical trial data for a once weekly long-acting insulin called insulin icodec by Novo Nordisk.
If this insulin is approved for patients by the Food and Drug Administration (FDA), it would be transformational because other long-acting insulins such as insulin glargine (also known as Lantus, Basaglar, or Toujeo) and insulin degludec (also known as Tresiba) require daily injections.
Insulin icodec would be the first option that allows a once weekly injection, decreasing the number of weekly injections from seven to one!
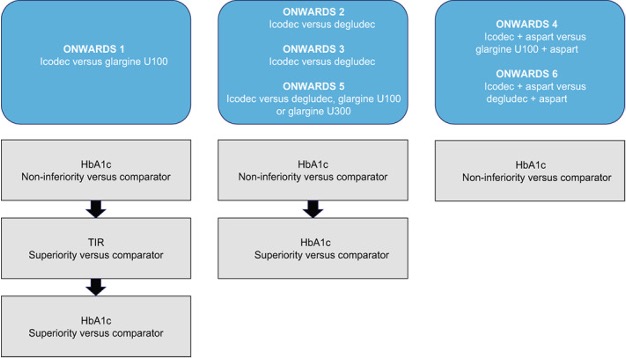
I’ll provide a brief overview of results from three studies including the ONWARDS 1, 3, and 4 trials. All the studies used reduction in Hemoglobin A1c (HbA1c), a measure of average blood glucose over the past two to three months, to evaluate effectiveness.
The ONWARDS 1 trial compared insulin icodec to insulin glargine. The study was conducted with patients who had not received insulin before. It was determined that patient’s HbA1c reduced from 8.5% to 6.93% with the new insulin icodec compared to a reduction from 8.44% to 7.12% with insulin glargine. Furthermore, patients who received insulin icodec spent more time in their target blood glucose range compared to insulin glargine.
In the ONWARDS 3 trial, insulin icodec was compared to insulin degludec. The patients in this study also included patients who had not used insulin before. The results from this trial demonstrated similar effectiveness for both insulins in terms of HbA1c and fasting blood glucose reduction.
The last study I want to highlight is the ONWARDS 4 trial. Insulin icodec was compared to insulin glargine for type 2 diabetics with long-standing type 2 diabetes. The patients in this trial were on a basal-bolus insulin regimen which means they managed their diabetes with short and long-acting insulins. It was found that both insulins resulted in similar reductions of HbA1c. The two insulins also had similar safety profiles with no new safety concerns for insulin icodec.
In summary, insulin icodec would provide a significantly more convenient administration option for patients who qualify for a long-acting insulin to manage their diabetes. It may allow you to inject insulin only once a week and provides similar effectiveness and safety as highlighted by the trials I mentioned above.
Therefore, with potential FDA approval coming in 2024, I encourage you to have a conversation with your doctor if insulin icodec sounds like an interesting option for you.
Feel free to use the resources linked below to learn more as there is also a trial called ONWARDS 6 that is studying the new insulin in Type 1 diabetics!
References:
- Rationale and design of the Phase 3A Development Programme (onwards 1-6 trials) investigating once-weekly insulin icodec in diabetes. Diabetes, obesity & metabolism. October 14, 2022. Accessed July 12, 2023. https://pubmed.ncbi.nlm.nih.gov/36106652/.
- Lingvay I, Asong M, Desouza C, et al. Once-weekly insulin Icodec vs once-daily insulin degludec in adults with insulin-naive type 2 diabetes. JAMA. Published online June 24, 2023. doi:10.1001/jama.2023.11313
- Mathieu C, Ásbjörnsdóttir B, Bajaj HS, et al. Switching to once-weekly insulin icodec versus once-daily insulin glargine U100 in individuals with basal-bolus insulin-treated type 2 diabetes (onwards 4): A phase 3a, randomised, open-label, multicentre, treat-to-target, non-inferiority trial. The Lancet. 2023;401(10392):1929-1940. doi:10.1016/s0140-6736(23)00520-2
- Rosenstock J, Bain SC, Gowda A, et al. Weekly ICODEC versus daily glargine U100 in type 2 diabetes without previous insulin. New England Journal of Medicine. Published online June 24, 2023. doi:10.1056/nejmoa2303208